Continued Evolution of ESF Concepts
by IMEX Veterinary
Since the 1980’s, external skeletal fixation has become an increasingly popular method of veterinary fracture repair. Over that same time period, one can follow a steady progression away from simple ESF frames toward more complex ESF frames, often utilizing multiple external rods and full-pins. For those of us who’s early external fixation experience was based on simple frames with smooth pins, the evolution to complex frames with threaded pins was a blessing. No longer would so many of our patients suffer from poor limb use and premature pin loosening. Evolution to complex frames with positive threaded pins was based on clinical experience and mechanical testing, and assisted in revitalizing the use of ESF. With more consistent, repeatable clinical success, practitioners became willing to utilize external fixation on more and more fractures, not just on open, contaminated injuries.
With the evolution of more stable frame constructs utilizing positive-profile threaded pins, application of the KE device became more and more time consuming, hardware intensive, and expensive. However, time and effort put into building complex frames and targeting pins yielded such improved clinical performance that “modern” ESF concepts were widely accepted and applied. Mechanical aspects of these “modern” concepts included: utilize full-pins whenever possible; complex frames decrease morbidity; and stack or augment external rods whenever full-pins are not used. Development of acrylic and pin external fixators, utilization of full-pin aiming devices, availability of rod augmentation systems, and development of ESF clamps that could be added after the fact, were additional developments that somewhat simplified the application of “modern” ESF constructs.
Simple half-pin frames are the most powerful way to simplify the ESF technique
IMEX Veterinary, Inc. developed the SK ESF system to address the limitations and frustrations associated with the KE device. Design criteria for the SK ESF clamp included the ability to effectively grip a wide range of different pin diameters, capacity to pass positive threaded pins directly through the clamp bolt, ability to add or subtract a pin or clamp after the fact, independence from expensive instrumentation to apply fixation pins and frames, and the capability of the clamp to act as an aiming device. Such design criteria facilitates the construction of “modern” ESF frames regardless of their degree of complexity.
FIGURES 2 and 3 | Mechanical testing of Type I-a frames demonstrates that the traditional external rod is the weak link. Bending of the rod is not usually permanent, but results in premature pin loosening and poor limb function. Complex frames can hide weak rods. Strong rods are mandatory to achieve simple but strong frames. (See “Bending Stiffness Comparison of External Rods” chart shown below, which contains previously collected data.)
Fractured Tibia/Fibula
1.5-year-old, intact, male Chocolate Lab
Grade I, Open Tibial Fracture
18-month-old, intact, male Airedale
Tibial Fracture
1-year-old, intact, male German Shepherd, 40 kg

FIGURE 8 | 6-week radiograph demonstrating excellent fracture healing. The fixator was removed at this time.

FIGURE 9 | Gross photo of patient 18 hours postoperatively.
Severe Metatarsal Valgus Deformity
1-week-old thoroughbred foal
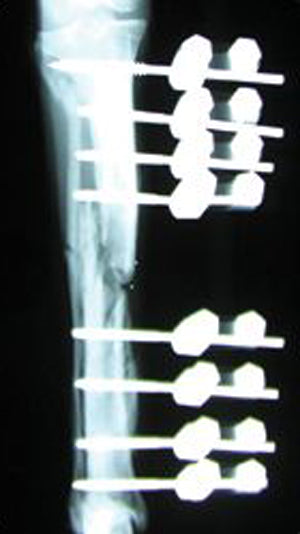
FIGURES 10 and 11 | Thoroughbred foal presented at 1 week of age with severe metatarsal valgus deformity. Foal was walking on lateral aspect of metatarsophalangeal joint, causing a large soft tissue wound that made traditional plating methods less than ideal. A wedge osteotomy was performed and a Type III, large SK ESF device was applied to stabilize the osteotomy and reduction. The foal went to union and device removal. A recheck at 8 months of age showed the foal walking well.
However, the most powerful way to simplify the ESF method lies in mechanical frame improvements that are not dependent on complex frames for consistent and predictable clinical success. It has been shown that with the KE device, the external rod is the weak link in simple frame constructs (see figures 1, 2, and 3). To overcome the mechanical weakness of the KE device, surgical techniques evolved to the use of complex frames. While most new ESF devices have been designed to simplify construction of complex frames, the SK ESF system is the first veterinary ESF device to recommend and mechanically support simpler frame constructs.
While simplifying frame construction, the SK ESF system also addresses the weak rod problem with connecting rods that are significantly larger in diameter than those historically used in veterinary medicine. With external rods no longer being such a weak link, it is not necessary to build complex frames or to incorporate full-pins to achieve frame strength. In fact, a simple study of frame stiffness comparing common frame geometries of the medium KE and the large SK frames (both with identical pin number and pin size) was performed to further outline the ramifications of incorporating more rigid external rods into ESF frames (Bronson, D.G., Ross, J.D., Welch, R.D., Proceedings of Veterinary Orthopedic Society Annual Meeting, 1999). Results of that study indicate that the large SK Type I-b provides 60% of the axial strength of the most complex Type III KE frame. In cranio-caudal bending the simplest Type I-a, large SK frame exceeds all KE frames except the Type III. Comparable Type I-a and Type I-b frames exhibit a 4-fold increase in stiffness when constructed utilizing large SK rods instead of medium KE rods.
As one can see, by utilizing the strong external rods of the SK fixator, one can expect simple frame constructs to perform without loss of mechanical integrity. Since introduction of the SK system in 1998, our customers utilizing the SK fixator have progressively gained confidence in utilizing simple SK frames instead of the typical, more complex frames required with KE components.
Simple half-pin frames are the most powerful way to simplify the ESF technique because:
Prior to introduction of the SK system, we encouraged customers to build the complex frames necessary at that time for consistent, repeatable clinical success. Since 1998 we have encouraged customers to evolve away from the KE mentality of frame construction and instead to rely on simple Type I-a, Type I-b, and occasionally minimal Type II frames (only one full-pin per segment) when necessary. Customers utilizing appropriate sized SK fixators continue to gain confidence in utilizing simpler frames instead of the more complex frames necessitated with the KE and KE like fixators. In fact, the SK fixator is the only fixator to recommend use of simpler half-pin based frames over more complex frame geometries.
However, should a particularly challenging case be presented, the SK ESF system can easily be configured to any degree of complexity necessary.
If you are using the SK fixator with a Kirschner-Ehmer mentality, please consider giving some thought to two things:
Most importantly, the SK ESF system provides the veterinary surgeon an opportunity to simplify the ESF method to a greater degree than with other ESF devices. This simplification is provided not only by the user-friendly nature of the SK clamp, but most importantly by the structural properties of the SK external connecting rods. Without a planned destabilization strategy, complex frames with full-pins may be contraindicated using the SK ESF System.
In summary, the case examples presented in this issue of the IMEX Update are not exceptions, but represent the design philosophy of the SK ESF system in action. Surgeons experienced with the KE and newer KE like devices would not (and should not) utilize the simple frames shown in this article. Likewise, it would be acceptable in cases 1 and 3 to have utilized Type I-b or minimal Type II frames with a potential for staged disassembly. The equine case serves to demonstrate that complex frames can readily be applied using the SK ESF system, but are likely too strong for use in most canine patients. It may take some time and experience to gain confidence with a fixation system designed to perform with relatively simple frame constructs; however, frame cost, surgical time, and patient morbidity can all be reduced by utilizing them.